Periodontics Specialist
Louis C. Franzetti, DDS
Dentist & Periodontist located in Manhattan, New York, NY
Dr. Franzetti is an expert in non-surgical periodontics treatments aimed at preventing and treating early- and late-stage gum disease in his patients from Manhattan, NY.
Periodontics Q & A
What is periodontics?
Periodontics is the specialty of dentistry that is responsible for the diagnosis, treatment and prevention of gum diseases and the surgical placement of implants.
Periodontal Disease
What is Periodontal Disease?
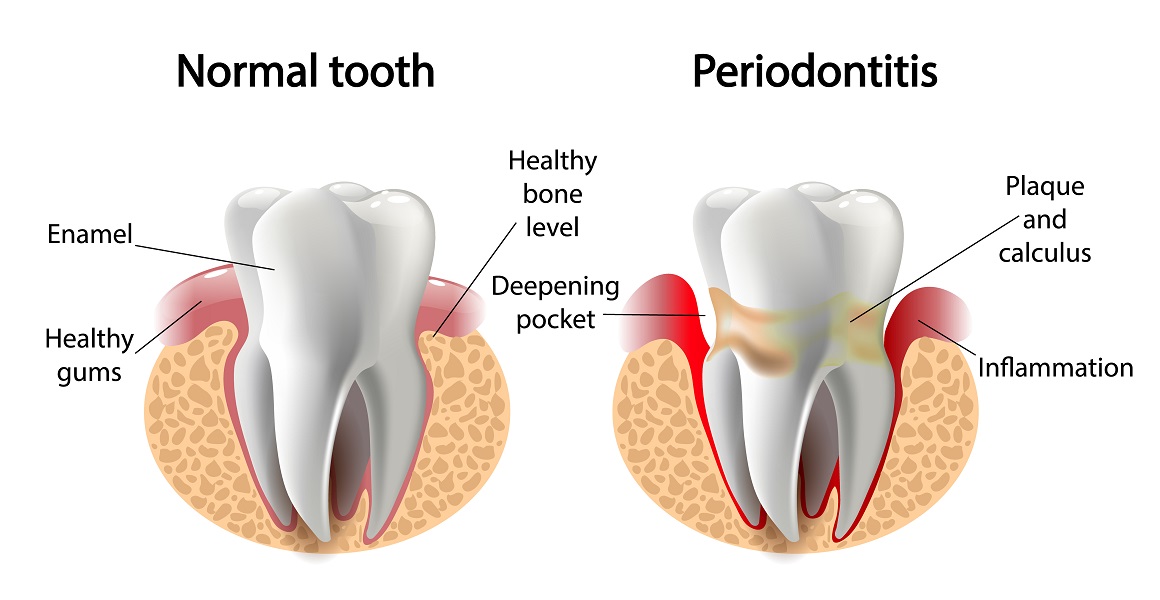
Periodontal diseases are a group of infections causing inflammation and destruction of the gum tissue and bone that surround and support teeth. Periodontal Diseases are divided into 2 main categories:
- Gingivitis
- Periodontitis
Gingivitis
The Stage 1 of gum disease is called Gingivitis. It is the inflammation of the superficial gum tissues and is reversible. Failure to regularly brush, floss and have professional tooth cleanings will cause the accumulation of plaque bacteria to build up between the gums & teeth.
Signs of Gingivitis
- Gums are tender and painful
- Gums are red or swollen
- Gums bleed after brushing / flossing.
Periodontitis
Gingivitis will most often progress into Periodontitis (bone loss) if left untreated.
The bacterial plaque spreads and grows below the gum line. Toxins produced by the bacteria will stimulate your body to develop a chronic inflammatory response. This inflammation will destroy gum tissue and bone. The result of this bone loss causes the formation of spaces around the teeth called Periodontal Pockets.
Advanced periodontitis
As pockets continue to deepen, the bacterial levels increase and cause severe bone and gum tissue loss. Teeth have now lost their bone support. They become mobile (lose) and are at risk of being lost. Additional complications including a heightened risk for heart disease, diabetes, stroke, and pre-term low weight babies are well documented.
A recent CDC report provides the following data related to the prevalence of Periodontitis in the U.S.
- 47.2% of adults aged 30 years and older have some form of periodontal disease.
- Periodontal disease increases with age, 70.1% of adults 65 years and older have periodontal disease.
This condition is more common in men than women (56.4% vs 38.4%), those living below the federal poverty level (65.4%), those with less than a high school education (66.9%), and current smokers (64.2%).
Warning signs
The following are some warning signs of periodontal disease:
- Bad breath or bad taste that won’t go away
- Red or swollen gums
- Tender or bleeding gums
- Painful chewing
- Loose teeth
- Sensitive teeth
- Gums that have pulled away from your teeth
- Any change in the fit of partial dentures
Risk factors
Certain factors increase the risk for periodontal disease:
- Smoking
- Diabetes
- Lack of consistent professional tooth cleaning visits
- Poor oral hygiene
- Stress
- Heredity
- Crooked teeth
- Underlying immuno-deficiencies—e.g., AIDS
- Fillings that have become defective
- Taking medications that cause dry mouth
- Bridges that no longer fit properly
- Female hormonal changes, such as with pregnancy or the use of oral contraceptives
What is the recommended care for Periodontal Disease?
Prevention
The cornerstone of successful periodontal treatment starts with establishing consistent oral hygiene techniques. This includes twice-daily brushing (at minimum) and daily interdental cleaning with floss and/or interdental brushes. For smaller spaces, products such as narrow soft-picks with gentle rubber bristles provide excellent manual cleaning. The use of an antiseptic mouth rinse (like Listerine) is also helpful. Persons with dexterity problems, such as arthritis, may find oral hygiene techniques too difficult. The use of an electric toothbrush and more frequent professional cleaning is advised.
Patients with Periodontitis must realize that it is a chronic inflammatory disease. In order to keep these affected teeth long-term, they must develop a lifelong regimen of meticulous oral hygiene and professional maintenance cleanings in a Periodontal specialty office.
Treatment
Phase 1: Initial therapy
Initial Therapy consists of:
-
Scaling and Root Planing (SRP)
SRP is the non-surgical removal of microbial plaque and calculus (tartar) 360 degrees around each tooth. Scaling removes bacterial deposits above the gumline while Root Planing removes deposits below the gumline. This procedure involves the use of specialized curettes and ultrasonic instruments to mechanically remove the plaque and calculus deposits. Initial therapy usually requires local anesthesia (Novocain) and may take multiple visits to adequately complete.
-
Local drug delivery
Local drug deliveries in Periodontology have gained acceptance and popularity compared to systemic drugs due to decreased risk of development of resistant flora and other side effects.] A meta-analysis of local tetracycline found improvement.
- Fix all broken fillings. It is important to close the contacts in between teeth to prevent food from getting lodged or caught between teeth.
- Check for any root canal problems
- Place any provisional (temporary) crowns or bridges
- Adjust the occlusion (bite) to prevent excessive force on teeth that have reduced bone support.
- Remove failing, non-restorable teeth with bone grafting to prepare the site for a future dental implant tooth replacement.
Reevaluation
The Periodontist must perform a re-evaluation 4 to 6 weeks after the initial scaling and root planning to determine if the patient’s oral hygiene has improved and inflammation has regressed sufficiently.
Non-Surgical scaling and root planing are usually successful when periodontal pockets are shallower than 4-5mm.
Pocket depths greater than 5–6 mm, which remain with bleeding upon probing, may indicate continued disease activity. This will very likely lead to further bone loss over time.
This is especially true in molar tooth sites where bone loss between the roots (furcation’s) has already begun.
Phase 2: Surgical Therapy
The scope of Dental (and Periodontal) Surgical therapy is a vast and complex topic.
Our explanation will attempt to give patients a clearer understanding of general surgical concepts and different modalities used to achieve specific goals all designed to create and maintain patients’ oral/periodontal health.
Concept #1:
All surgical procedures (after anesthesia) start with the gentle separation or reflection of the gum tissue away from the teeth or bone ridge. We don’t “cut gum tissue away” indiscriminately.
This reflection of tissue gives the surgeon access and visibility to remove all the infection at the junction of the tooth with bone or access to a healed bone ridge.
Concept #2:
Once access and visibility have been achieved, there are several options now possible depending upon the requirements dictated by careful examination and diagnoses.
- Bone grafting around teeth: to regenerate lost bone around teeth or implants.
- Bone grafting: to build up a ridge.
- Bone grafting sockets of extracted teeth.
- Gum grafts: to repair recessions of the gum around teeth.
- Crown Lengthening procedures: A crown lengthening is performed when there is very little remaining tooth structure. The procedure involves the removal of bone and soft tissue to expose more tooth surfaces so that they may be properly restored.
Periodontal surgery includes all the surgical techniques used to help treat or prevent gum disease. Gum disease is the most common cause of permanent tooth loss in the U.S. While some early or mild forms may be treated non-surgically, some types of advanced gum disease require more intensive approaches including periodontal surgery to restore gums, remove bacteria and tartar, and prevent permanent tooth loss.
If nonsurgical therapy is found to have been unsuccessful in managing signs of disease activity, periodontal surgery may be needed to stop progressive bone loss and regenerate lost bone where possible. Many surgical approaches are used in the treatment of advanced periodontitis, including open flap debridement and osseous surgery, as well as guided tissue regeneration and bone grafting. The goal of periodontal surgery is access to definitive calculus removal and surgical management of bony irregularities which have resulted from the disease process to reduce pockets as much as possible. Long&term studies have shown, in moderate to advanced periodontitis, surgically treated cases often have a less further breakdown over time and, when coupled with a regular post-treatment maintenance regimen, are successful in nearly halting tooth loss in nearly 85% of diagnosed people


